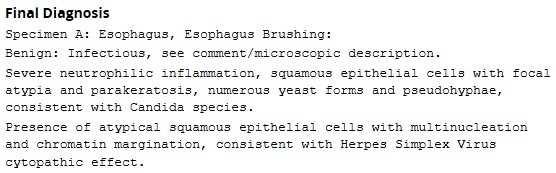
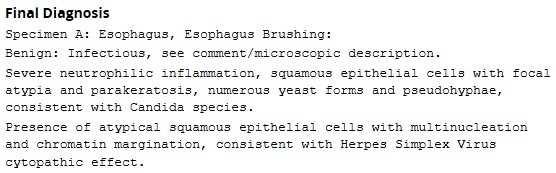
Case 2: A 35-Year-Old Woman with Melena
This 35-year-old woman presents to the ED with a three day history of melena. She reports daily methamphetamine use, and significant alcohol intake. She undergoes an upper endoscopy, which revealed the following adherent exudates in her esophagus, which cannot be washed off with water. What explains this finding, and what further testing should be performed?


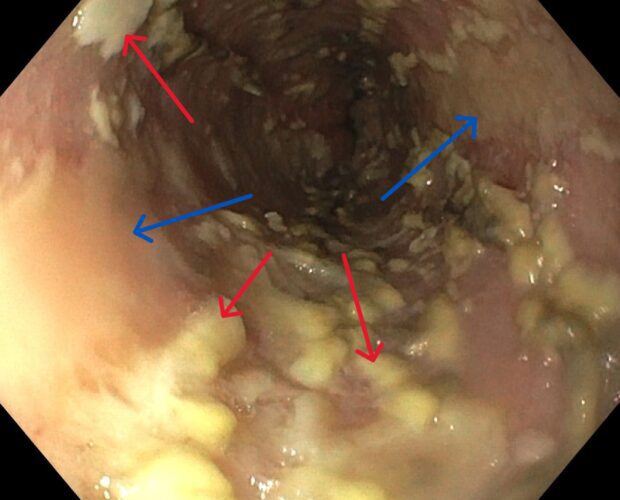
This patient has evidence of severe esophageal candidiasis (red arrows), and esophagitis (blue arrows).
Esophageal candidiasis is the most common type of infectious esophagitis, with immunocompromised patients (ex. HIV, leukemia, diabetes, corticosteroid use) being at the highest risk. Thus, its discover on endosopy should prompt testing for HIV. Other independent risk factors include frequent antibiotic use, and esophageal motility disorders. Patients frequently present with dysphagia, odynophagia, and retrosternal pain. On physical exam, oral thrush is often present, and the exudative lesions characteristically cannot be washed away with water.
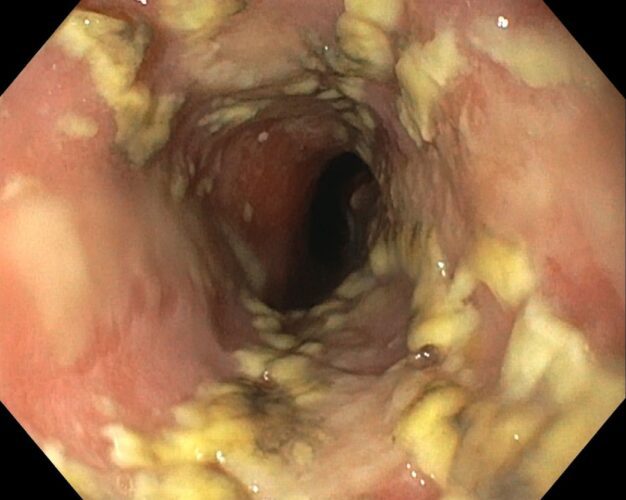
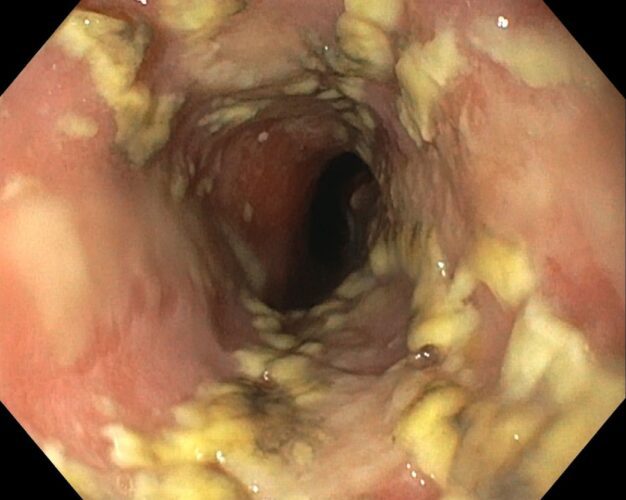
A confirmatory diagnosis is made with biopsy or brushings, which demonstrate yeast and pseudohyphae invading mucosal cells.
Source: Mohamed AA, Lu XL, Mounmin FA. Diagnosis and Treatment of Esophageal Candidiasis: Current Updates. Can J Gastroenterol Hepatol. 2019 Oct 20;2019:3585136. doi: 10.1155/2019/3585136. PMID: 31772927; PMCID: PMC6854261. Available from: https://pubmed.ncbi.nlm.nih.gov/31772927/
Her initial bloodwork returned positive for HIV, with a CD4 count of 19:
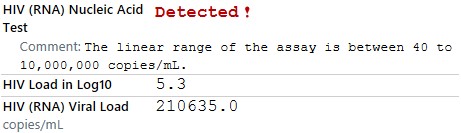
One week later, the pathology results from her esophageal brushing returned, revealing concurrent candidal and HSV esophagitis. An oral HSV NAT was also positive for HSV-1.