Case 1: A 74-Year-Old Woman with Ovarian Cancer
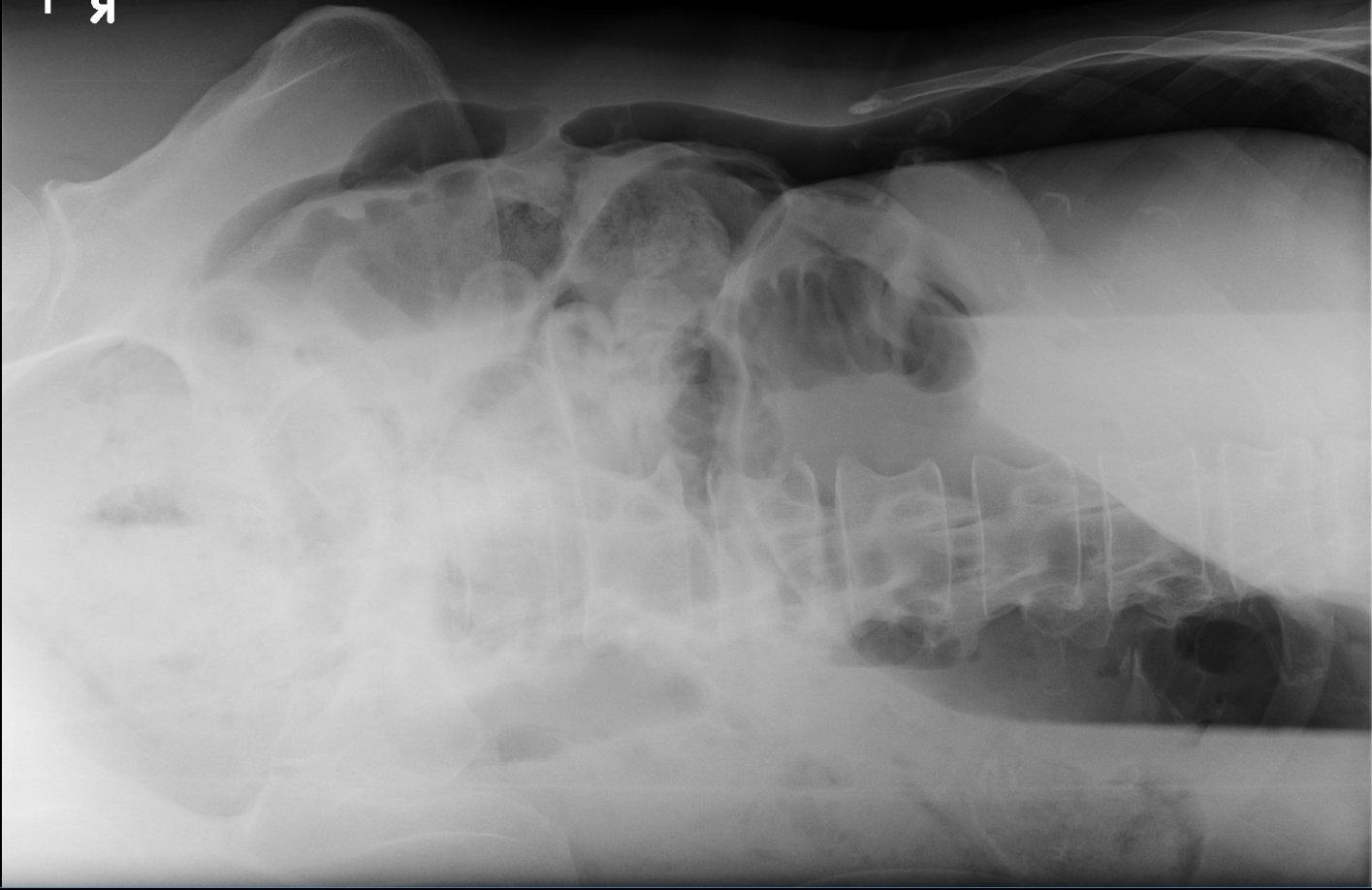
This 74-year-old woman has a history of moderate cognitive impairment, and was recently diagnosed with metastatic ovarian cancer. She presents to the emergency department via EMS after her husband returned home to find her lying on the floor, moaning and confused. A chest radiograph reveals the following:
![]()
![]()
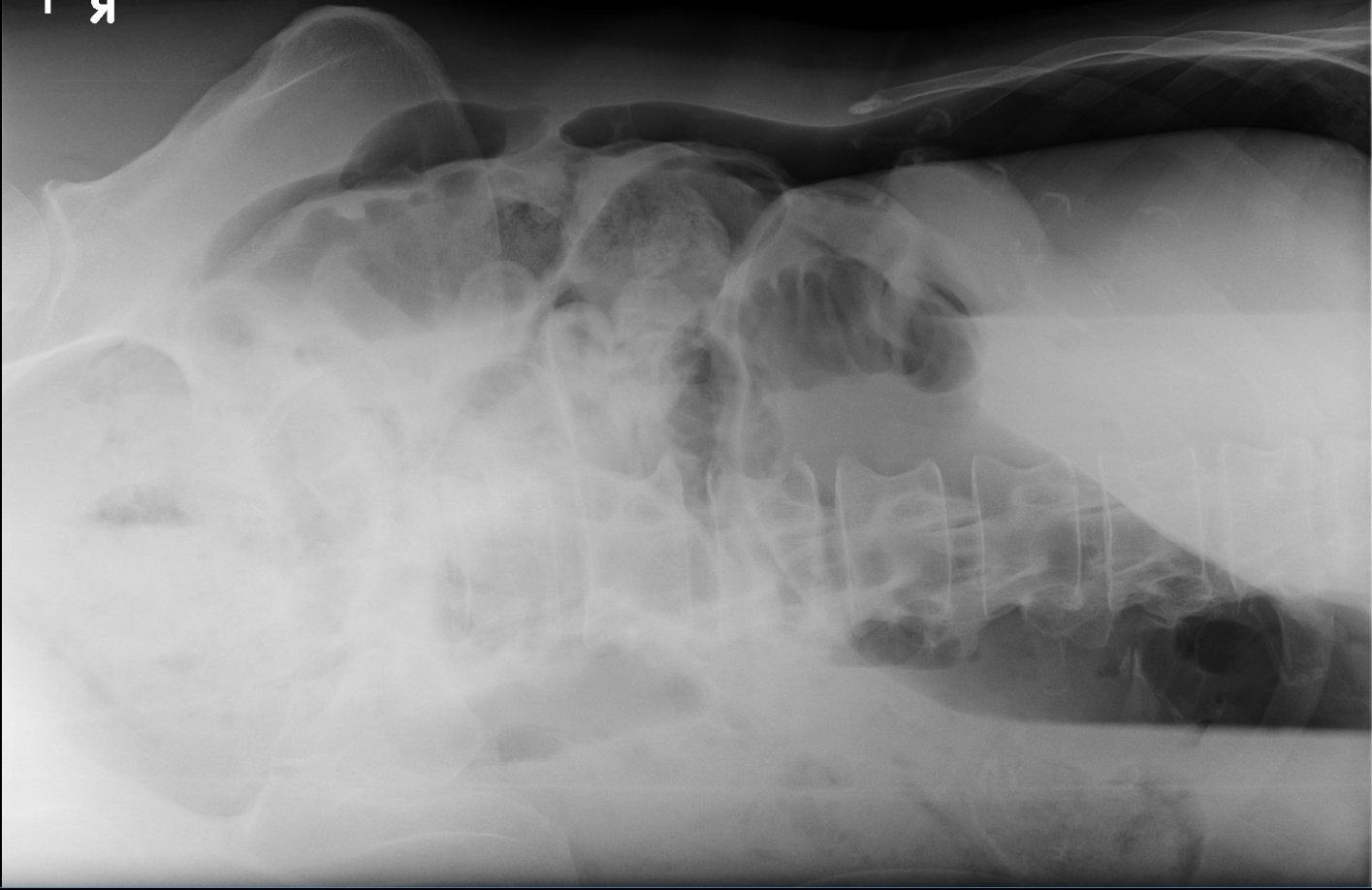
This chest radiograph demonstrates evidence of abdominal free air (pneumonoperitoneum), which is likely secondary to hollow viscus perforation related to her known ovarian cancer.
A gastrointestinal perforation occurs when a breach through all the layers of the bowel occurs, resulting in the escape of bowel contents into the peritoneal cavity. Patients typically present with abdominal pain and distention, vomiting, tachycardia, hypotension, and tachypena.
X-ray typically detects pneumoperitoneum with a sensitivity of 50-98%, dependent on the position of the patient (erect, supine, lateral decubitus). Smaller amounts of free air can however be missed, and are often detected on CT. Features on this xray to suggest pneumoperitoneum include subdiaphragmatic free air (red arrow), as well as air outlining both sides of the digestive lumen (blue arrows).
![]()
![]()
Source: Bansal J, Jenaw RK, Rao J, Kankaria J, Agrawal NN. Effectiveness of plain radiography in diagnosing hollow viscus perforation: study of 1,723 patients of perforation peritonitis. Emerg Radiol. 2012 Apr;19(2):115-9. doi: 10.1007/s10140-011-1007-y. Epub 2011 Dec 6. PMID: 22143167. Available from https://pubmed.ncbi.nlm.nih.gov/22143167/
Sureka B, Bansal K, Arora A. Pneumoperitoneum: What to look for in a radiograph? J Family Med Prim Care. 2015 Jul-Sep;4(3):477-8. doi: 10.4103/2249-4863.161369. PMID: 26288798; PMCID: PMC4535122. Available from https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4535122/#:~:text=Pneumoperitoneum%20is%20the%20presence%20of,on%20computerized%20tomography%20(CT).
An emergent abdominal xray was performed in both the AP and lateral views, which confirmed the diagnosis of pneumoperitoneum:


As perforations are surgical emergencies, their rapid detection and management is imperative.
In this case, the patient was sent for an emergent OR, and her perforation was localized and managed with a palliative illeostomy.