Case 25: A 73-Year-Old Man with Dysphagia
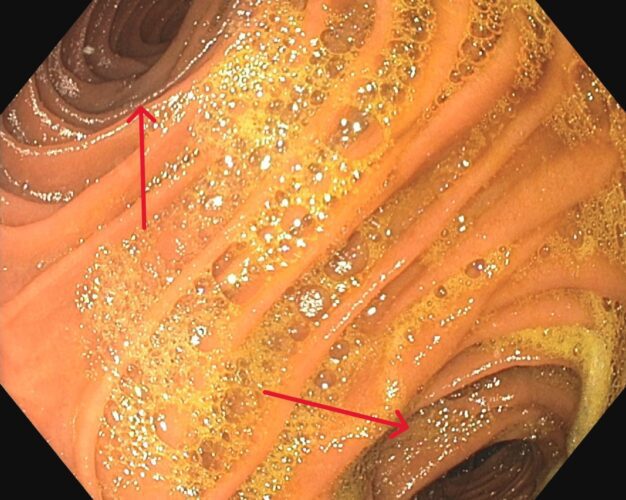
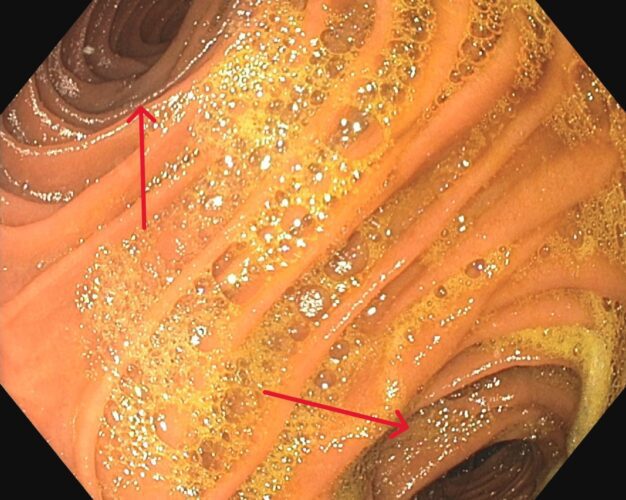
This 73-year-old man with a history of hypertension, dyslipidemia, and obesity with a previous bariatric surgery was referred to gastroenterology for a one-year history of dysphagia to solids and liquids. An upper endoscopy was performed, and the following bifurcation was noticed shortly after passing through the gastroesophageal junction. What explains this anatomical finding?
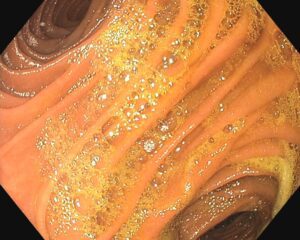
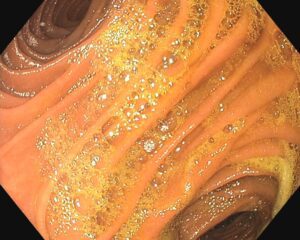
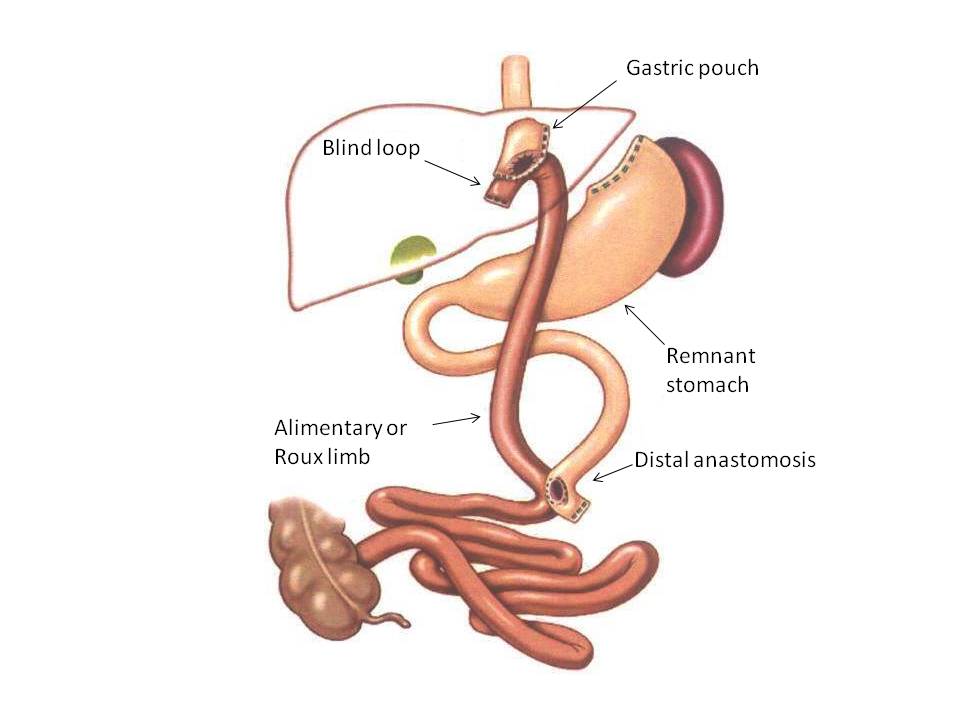
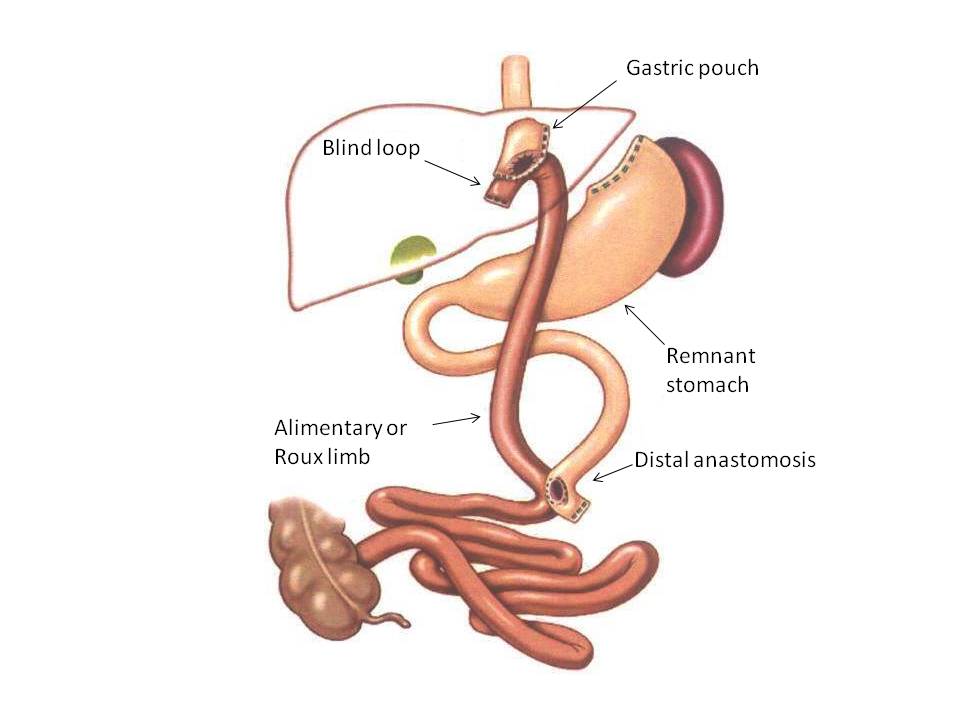
A review of the patients surgical record established that he had underwent a Roux-en-Y gastric bypass. As shown in the figure below, the procedure involves a gastrojejunostomy, where an end-to-side anastomosis is created to connect the end of the gastric pouch to the side of the jejunum. During an EGD, this anastomosis will appear as a double-barrel view when examined through the gastric lumen (red arrows). Whether the blind end of the jejunum faces the spleen or the liver is irrelevant, and is not decipherable endoscopically. However, the length of the blind end should be short (1 to 2 cm), because a longer blind end can lead to the lodging of food particles in what is referred to as ‘candy cane limb syndrome’, leading to patients presenting with nausea, vomiting, and abdominal pain. During endoscopy, it is important to be cautious when accessing this blind pouch, because the jejunum wall is thin and can be easily perforated.